More About How To Get Into A Pain Clinic In Ohio
If you live with chronic pain, you likely require a team of doctors to accomplish an optimum outcome. Here's what to anticipate from a discomfort specialized practice or center. So you've decided it's time to make a consultation with a discomfort physician, or at a pain center. Here's what you require to know before scheduling your visitand what to expect once you exist.
" Discomfort physicians come from various academic backgrounds," says Dmitry M. Arbuck, MD, president and medical director of the Indiana Polyclinic in Indianapolis, a discomfort management center. Dr. Arbuck is accredited by the American Academy of Discomfort Management and the American Board of Psychiatry and Neurology. "Any doctor from any specialtyfor instance, emergency medication, household practice, neurologymay be a pain doctor." The pain doctor you see will depend upon your symptoms, diagnosis, and needs.
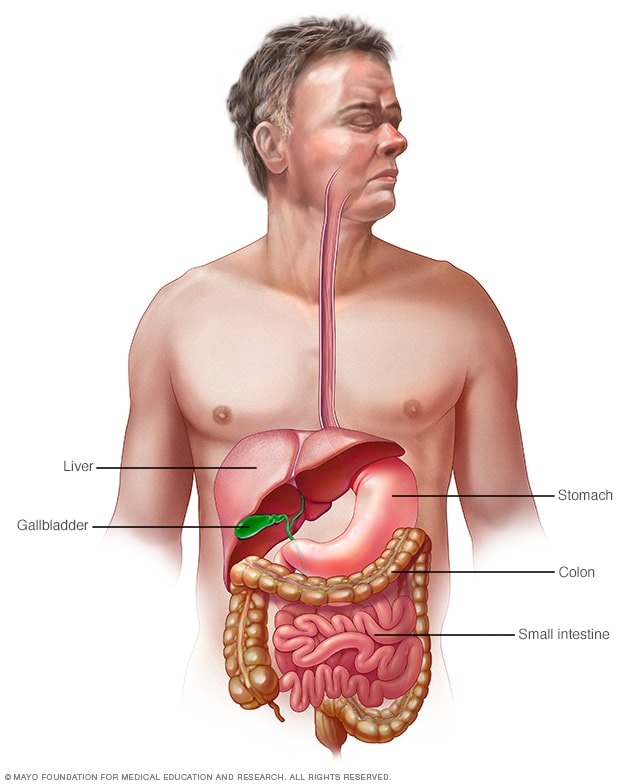
Arbuck explains - how to refer to a pain clinic. "The doctors within a discomfort management clinic or practice may focus on rheumatology, orthopedics, gastroenterology, psychiatry," or other areas, for instance. Pain doctors have actually earned the title of MD (Physician of Medication) or DO (Medical Professional of Osteopathic Medicine). Some pain physicians are fellowship-trained, implying they received post-residency training in this sub-specialty.
( Learn more about interventional pain methods.) Pain physicians who have actually met specific qualificationsincluding completing a residency or fellowship and passing a composed examare considered to be board-certified. Many pain physicians are dual-board certified in, for instance, anesthesiology and palliative medication. However, not all pain physicians are board-certified or have formal training in discomfort medicine, but that does not mean you shouldn't consult them, states Dr.
Dr. Arbuck suggests that people looking for help for persistent pain see doctors at a clinic or a group practice because "no one professional can actually treat discomfort alone." He discusses, "You don't want to select a particular type of doctor, always, however a good doctor in a good practice."" Discomfort practices ought to be multi-specialty, with a good credibility for using more than one strategy and the ability to attend to more than one issue," he recommends.
As Dr. Arbuck describes, "If you have one physician or specialty that's more vital than the others," the therapy that specialty prefers will be emphasized, and "other treatments may be disregarded." This model can be bothersome due to the fact that, as he explains: "One discomfort client may require more interventions, while another might require a more psychological technique." And because discomfort clients also gain from multiple therapies, they "require to have access to doctors who click here can refer them to other professionals along with work with them." Another benefit of a multi-specialty pain practice or clinic is that it helps with routine multi-specialty case conferences, in which all the physicians meet to discuss client cases.
Some Known Factual Statements About What Disease Is The Estimated Cost For A Free-standing Pain Clinic
Arbuck explains. Think of it like a board meetingthe more that members with various backgrounds collaborate about an individual challenge, the more most likely they are to resolve that specific problem. At a discomfort center, you may likewise satisfy with occupational therapists (OTs), physical therapists (PTs), certified doctor's assistants (PA-C), nurse professionals (NPs), licensed acupuncturists (LAc), chiropractic practitioners (DC), and exercise physiologists.

The latter are typically social employees, with titles such as licensed medical social worker (LCSW). Dr. Arbuck views reliable pain medicine as a spectrum of services, with mental treatment on one end and interventional discomfort management on the other. In in between, patients have the ability to obtain a mix of pharmacological and rehabilitative services from different medical professionals and other doctor.
Preliminary visits may include one or more of the following: a physical examination, interview about your case history, pain evaluation, and diagnostic tests or imaging (such as x-rays). In addition, "A good multi-specialty clinic will pay equal attention to medical, psychiatric, surgical, household, dependency, and social history. That's the only method follow this link to evaluate patients thoroughly," Dr - where north of boston is there a pain clinic that accepts patients eith no insurance.
At the Indiana Polyclinic, for instance, clients have the chance to consult experts from four main locations: This might be an internist, neurologist, household professional, or perhaps a rheumatologist. This doctor normally has a large understanding of a broad medical specialized. This medical professional is most likely to be from a field that where interventions are frequently utilized to treat discomfort, such as anesthesiology.
This service provider will be someone who focuses on the function of the body, such as a physical medication and rehab (PM&R) physician, physiotherapist, physical therapist, or chiropractic practitioner. Depending on the client, he or she may likewise see a psychiatrist, psychologist, and/or psychotherapist. how to open a pain management clinic in florida. The client's medical care doctor may coordinate care.
Arbuck. "Narcotics are simply one tool out of many, and one tool can not operate at all times." Additionally, he notes, "pain clinics are not simply puts for injections, nor is pain management just about psychology. The objective is to come to consultations, and follow through with rehab programs. Pain management is a commitment.
Fascination About Where Is The Pain Clinic In Morristown
Arbuck mentions. Treatment can be pricey and because of that, patients and medical professional's workplaces often require to eliminate for medications, appointments, and tests, but this difficulty occurs outside of discomfort centers too. Clients should likewise be aware that anytime managed substances (such as opioids) are included in a treatment strategy, the doctor is going to request drug screenings and Patient Agreement types relating to rules to abide by for safe dosingboth are advised by federal agencies such as the FDA (see a sample Patient-Prescriber Opioid Agreement at https://www.fda.gov/media/114694/download).
" I didn't http://daltonmojn822.fotosdefrases.com/some-known-incorrect-statements-about-what-gets-you-kicked-out-of-a-pain-clinic just have pain in my head, it was in the neck, jaw, absolutely all over," recalls the HR expert, who lives in the Indianapolis location. Wendy started seeing a neurologist, who put her on high doses of the anti-seizure medications gabapentin and zonisamide for pain relief. Unfortunately, she says, "The discomfort worsened, and the adverse effects from the medication left me unable to functionI had amnesia, blurred vision, and muscle weakness, and my face was numb.
Wendy's neurologist provided her Botox injections, but these triggered some hearing and vision loss. She likewise tried acupuncture and even had a discomfort relief gadget implanted in her lower back (it has given that been gotten rid of). Lastly, after 12 years of extreme, persistent discomfort, Wendy was referred to the Indiana Polyclinic.
She likewise went through different assessments, consisting of an MRI, which her previous medical professional had carried out, along with allergic reaction and hereditary screening. From the latter, "We learned that my system does not take in medication correctly and discomfort medications are not effective." Quickly afterwards, Wendy got some unexpected news: "I learnt I didn't have chronic migraine, I had trigeminal neuralgia." This condition provides with signs of severe pain in the facial location, triggered by the brain's three-branched trigeminal nerve.
Wendy started receiving nerve blocks from the clinic's anesthesiologist. She gets 6 shots of lidocaine (an anesthetic) and an anti-inflammatory to her forehead and cheeks. "It's five minutes of agonizing pain for four months of relief," Wendy shares. She also took the chance to work with the clinic's discomfort psychologist twice a month, and the occupational therapist once a month.
The Best Strategy To Use For How To Refer To A Pain Clinic
If you live with chronic pain, you likely need a team of physicians to attain an ideal result. Here's what to anticipate from a pain specialized practice or center. So you've decided it's time to make an appointment with a pain physician, or at a pain clinic. Here's what you require to know prior to scheduling your visitand what to expect once you exist.
" Pain physicians come from lots of different instructional backgrounds," states Dmitry M. Arbuck, MD, president and medical director of the Indiana Polyclinic in Indianapolis, a pain management clinic. Dr. Arbuck is licensed by the American Academy of Discomfort Management and the American Board of Psychiatry and Neurology. "Any doctor http://daltonmojn822.fotosdefrases.com/some-known-incorrect-statements-about-what-gets-you-kicked-out-of-a-pain-clinic from any specialtyfor circumstances, emergency medicine, family medicine, neurologymay be a discomfort doctor." The discomfort physician you see will depend on your symptoms, diagnosis, and requires.
Arbuck explains - what pain clinic will give you roxy 15th for back pain. "The doctors within a pain management clinic or practice might concentrate on rheumatology, orthopedics, gastroenterology, psychiatry," or other areas, for instance. Discomfort doctors have actually earned the title of click here MD (Medical Professional of Medicine) or DO (Medical Professional of Osteopathic Medicine). Some pain physicians are fellowship-trained, implying they got post-residency training in this sub-specialty.
( Learn more about interventional pain techniques.) Pain physicians who have satisfied specific qualificationsincluding completing a residency or fellowship and passing a written examare thought about to be board-certified. Many discomfort physicians are dual-board certified in, for example, anesthesiology and palliative medicine. However, not all discomfort physicians are board-certified or have official training in pain medicine, however that does not imply you shouldn't consult them, says Dr.
Dr. Arbuck recommends that individuals seeking help for persistent discomfort see physicians at a center or a group practice because "no one follow this link expert can actually treat discomfort alone." He discusses, "You do not desire to select a specific type of doctor, always, but an excellent doctor in an excellent practice."" Discomfort practices must be multi-specialty, with an excellent credibility for utilizing more than one method and the ability to resolve more than one problem," he encourages.
As Dr. Arbuck explains, "If you have one medical professional or specialized that's more important than the others," the treatment that specialty prefers will be emphasized, and "other treatments may be ignored." This design can be troublesome since, as he describes: "One discomfort client may require more interventions, while another might require a more psychological method." And due to the fact that pain clients also take advantage of numerous therapies, they "require to have access to physicians who can refer them to other specialists along with deal with them." Another advantage of a multi-specialty discomfort practice or clinic is that it facilitates routine multi-specialty case conferences, in which all the medical professionals satisfy to go over patient cases.
Getting My Clecveland Clinic How Do I Get Rid Of Shingle Pain To Work
Arbuck explains. Think of it like a board meetingthe more that members with different backgrounds team up about a specific challenge, the most likely they are to fix that specific issue. At a pain clinic, you might likewise consult with physical therapists (OTs), physiotherapists (PTs), licensed doctor's assistants (PA-C), nurse practitioners (NPs), licensed acupuncturists (LAc), chiropractic practitioners (DC), and exercise physiologists.
The latter are frequently social employees, with titles such as certified clinical social employee (LCSW). Dr. Arbuck views effective pain medicine as a spectrum of services, with psychological treatment on one end and interventional pain management on the other. In in between, patients are able to obtain a combination of pharmacological and rehabilitative services from various doctors and other doctor.
Preliminary consultations may consist of one or more of the following: a physical examination, interview about your case history, pain evaluation, and diagnostic tests or imaging (such as x-rays). In addition, "An excellent multi-specialty center will pay equal attention to medical, psychiatric, surgical, family, dependency, and social history. That's the only method to examine clients completely," Dr - clecveland clinic how do i get rid of shingle pain.
At the Indiana Polyclinic, for example, patients have the chance to seek advice from experts from 4 primary locations: This may be an internist, neurologist, family practitioner, or perhaps a rheumatologist. This medical professional usually has a large understanding of a broad medical specialty. This doctor is likely to be from a field that where interventions are typically used to treat discomfort, such as anesthesiology.
This supplier will be someone who specializes in the function of the body, such as a physical medication and rehab (PM&R) doctor, physical therapist, physical therapist, or chiropractic practitioner. Depending upon the patient, she or he might also see a psychiatrist, psychologist, and/or psychotherapist. what kind of ortho clinic do you see for hip pain. The patient's primary care physician might collaborate care.
Arbuck. "Narcotics are simply one tool out of many, and one tool can not work at perpetuity." Furthermore, he notes, "pain centers are not just places for injections, nor is pain management simply about psychology. The goal is to come to visits, and follow through with rehabilitation programs. Discomfort management is a dedication.
All About Who To Complain To About Pain Clinic
Arbuck mentions. Treatment can be expensive and because of that, clients and medical professional's offices frequently require to combat for medications, appointments, and tests, but this challenge takes place outside of pain clinics also. Clients need to also understand that anytime controlled substances (such as opioids) are included in a treatment strategy, the doctor is going to request drug screenings and Patient Agreement forms relating to guidelines to abide by for safe dosingboth are advised by federal agencies such as the FDA (see a sample Patient-Prescriber Opioid Arrangement at https://www.fda.gov/media/114694/download).
" I didn't just have discomfort in my head, it was in the neck, jaw, definitely everywhere," remembers the HR expert, who resides in the Indianapolis location. Wendy began seeing a neurologist, who put her on high doses of the anti-seizure medications gabapentin and zonisamide for discomfort relief. Unfortunately, she states, "The discomfort got worse, and the side results from the medication left me unable to functionI had memory loss, blurred vision, and muscle weak point, and my face was numb.
Wendy's neurologist offered her Botox injections, however these caused some hearing and vision loss. She also tried acupuncture and even had a pain relief gadget implanted in her lower back (it has actually because been removed). Lastly, after 12 years of serious, chronic pain, Wendy was described the Indiana Polyclinic.
She likewise underwent various evaluations, including an MRI, which her previous physician had carried out, in addition to allergy and hereditary testing. From the latter, "We learned that my system does not soak up medication properly and discomfort medications are ineffective." Soon afterwards, Wendy got some unexpected news: "I discovered I didn't have persistent migraine, I had trigeminal neuralgia." This condition presents with signs of severe pain in the facial location, triggered by the brain's three-branched trigeminal nerve.
Wendy started receiving nerve blocks from the clinic's anesthesiologist. She gets six shots of lidocaine (an anesthetic) and an anti-inflammatory to her forehead and cheeks. "It's 5 minutes of excruciating pain for four months of relief," Wendy shares. She also seized the day to deal with the clinic's pain psychologist twice a month, and the occupational therapist once a month.
Who Are The Pa's And Np's At Sanford Pain Clinic Can Be Fun For Anyone
Persistent arthritis pain can interfere with every element of life from work efficiency and everyday tasks, to getting quality rest and even personal relationships. clecveland clinic how do i get rid of shingle pain. If you can't get your pain under control regardless of treatment and healthy way of life routines, you may wish to consider attending a pain rehab program (PRP). where is northoaks pain management clinic. While discomfort centers can assist anybody with chronic discomfort, people with inflammatory types of arthritis and fibromyalgia might benefit the most from PRPs, says Daniel Clauw, MD, professor of anesthesiology https://www.google.com/maps/d/edit?mid=1WWfbdZZdAd2Jf0itJqwd0ZOMG_H_Ml8z&usp=sharing at the University of Michigan.


: Are one-stop stores where a https://www.google.com/maps/d/edit?mid=1GwOssZIKr2cMryvddGYRO-jgOIuofEYc&usp=sharing group of health professionals collaborates to help clients by utilizing a variety of evidence-based techniques. Programs that utilize an interdisciplinary approach are best, states Clauw, and might consist of physical and occupational therapists, psychologists, dietitians, nurses, https://www.google.com/maps/d/edit?mid=11vdMr66GB-_fNTml94_bEGrm7PDJTo6y&usp=sharing medical professionals and other healthcare providers. Offer procedures such as injections and nerve blocks - what pain clinic will give you roxy 15th for back pain. what are the policies for prescribing opiates in a pain clinic in ny.
How Does A Pain Management Clinic Help People Can Be Fun For Everyone
Chronic arthritis discomfort can disrupt every aspect of https://www.google.com/maps/d/edit?mid=1GwOssZIKr2cMryvddGYRO-jgOIuofEYc&usp=sharing life from work performance and everyday tasks, to getting quality rest and even personal relationships. who are the pa's and np's at sanford pain clinic. If you can't get your discomfort under control regardless of treatment and healthy lifestyle practices, you may desire to consider going https://www.google.com/maps/d/edit?mid=11vdMr66GB-_fNTml94_bEGrm7PDJTo6y&usp=sharing to a pain rehabilitation program (PRP). what is a pain management clinic https://www.google.com/maps/d/edit?mid=1WWfbdZZdAd2Jf0itJqwd0ZOMG_H_Ml8z&usp=sharing nhs. While discomfort centers can assist anybody with persistent discomfort, people with inflammatory kinds of arthritis and fibromyalgia may benefit the most from PRPs, states Daniel Clauw, MD, professor of anesthesiology at the University of Michigan.
: Are one-stop shops where a group of health professionals works together to assist patients by utilizing a variety of evidence-based approaches. Programs that use an interdisciplinary approach are best, states Clauw, and may include physical and physical therapists, psychologists, dietitians, nurses, physicians and other doctor. Deal procedures such as injections and nerve blocks - what was the first pain management clinic. how to set up a pain management clinic.

4 Simple Techniques For How To Set Up A Pain Management Clinic
Persistent arthritis discomfort can interfere with every aspect of life from work efficiency and day-to-day chores, to getting quality rest and even individual relationships. how to establish a pain management https://www.google.com/maps/d/edit?mid=1WWfbdZZdAd2Jf0itJqwd0ZOMG_H_Ml8z&usp=sharing clinic. If you can't get your pain under control despite treatment and healthy lifestyle routines, you might desire to consider going to a discomfort rehabilitation program (PRP). who are the doctors at eureka pain clinic. While pain clinics can assist anyone with chronic pain, individuals with inflammatory types of arthritis and fibromyalgia might https://www.google.com/maps/d/edit?mid=11vdMr66GB-_fNTml94_bEGrm7PDJTo6y&usp=sharing benefit the most from PRPs, states Daniel Clauw, MD, professor of anesthesiology at the University of Michigan.

: Are one-stop shops where a group of health professionals interacts to assist patients by using a variety of evidence-based approaches. Programs that https://www.google.com/maps/d/edit?mid=1GwOssZIKr2cMryvddGYRO-jgOIuofEYc&usp=sharing use an interdisciplinary technique are best, states Clauw, and may include physical and physical therapists, psychologists, dietitians, nurses, doctors and other doctor. Deal treatments such as injections and nerve blocks - how to get prescribed roxicodone from my pain clinic. how to get into a pain management clinic when pregnant.
The smart Trick of How Long Does It Take To Get An Appointment At A Pain Clinic That Nobody is Discussing
Considering that lots of kinds of chronic discomfort may need a complex treatment plan as well as specialized interventional methods, pain specialists today must have more training than in the past, and you ought to learn about how your pain physician was trained and whether he or she has board accreditation in discomfort management.
Most fellowship programs are associated with anesthesiology residency training programs. There are also fellowship programs associated with neurology and physical medicine and rehab residency programs. The fellowship includes a minimum of one year of training in all elements of discomfort management after conclusion residency training. When a physician has become board licensed in their primary specialized and has actually completed a recognized fellowship, they end up being qualified for subspecialty board accreditation in pain management by the American Board of Anesthesiology, The American Board of Psychiatry and The American Board of Neurology, or the American Board of Physical Medication and Rehabilitation.
In addition to finding out about your discomfort physicians training and board accreditation, you also need to ask whether they have experience with your specific discomfort condition and what types of treatments they offer (what i need for open a pain clinic office Drug Detox in ms). Do they only perform procedures or do they use a multidisciplinary method to discomfort management? Who do they describe for other treatment alternatives such as surgery, psychological support or alternative treatments? How can they be reached if questions or issues arise? What is their total philosophy of pain management? The finest method to be described a pain management specialist is through your medical care physician.
Rumored Buzz on How To Shut Down Pain Clinic
Patients are likewise typically referred by specialists who deal with various kinds of discomfort problems. Back surgeons, neurologists, cancer doctors, as well as other specialists generally work frequently with a discomfort doctor and can refer you to one. On your first visit to a discomfort management specialist, he or she will learn more about you and start to assess your particular discomfort issue.
The questions you are asked and the health examination will focus on your specific problem, however your pain doctor will need to know about previous and current medical history as well. Typically you will be provided a questionnaire prior to your very first see that will ask detailed questions about your pain problem, and you will probably be asked to bring any imaging studies (such as X-rays, computed tomography [CAT] scans, or magnetic resonance imaging [MRI] scans) or other tests that have actually currently been done.
If so, you might require a motorist to take you home. Most importantly, this visit is a chance for your discomfort doctor to begin to analyze all of this brand-new information and go over with you an initial evaluation of your pain problem. He or she may know exactly what is triggering your discomfort, or maybe additional diagnostic procedures will be needed.
An Unbiased View of What Happens At A Pain Management Clinic
A pain clinic is a health care resource that focuses on the diagnosis, management and treatment of chronic pain. Within lots of clinics, specialists that focus on different pain types and conditions are offered. A discomfort management expert is a doctor with extra training in the diagnosis and treatment of pain.

Pain management professionals recommend medications, carry out procedures (such as spinal injections and nerve blocks) and advise therapies to deal with discomfort. The very first visit to a discomfort management clinic typically involves a visit with a family doctor, internist, nurse professional or medical assistant. The visit generally involves a comprehensive assessment of the individual's pain history, a physical test, discomfort assessment, and diagnostic tests.
Depending on the origin and severity of persistent discomfort, a consultation for an assessment with a various pain expert within the center may be suggested. Physicians typically available at a pain clinic include the following: General PractitionersInternists NeurologistsRheumatologistsAnesthesiologistsOrthopedistsPhysiatristsPsychiatristsOther specialists at a discomfort center may include physical therapists, occupational therapists, chiropractors, acupuncturists and psychologists.
The 7-Minute Rule for What Are The Hours At The Pain Clinic In Pell City
These standards are for historical https://diigo.com/0iro50 reference just. IASP adopted the Recommendations for Pain Treatment Providers in May 2009. IASP thinks that clients throughout the world would benefit from the facility of a set of desirable characteristics for discomfort treatment facilities. The principles set forth in this document can work as a guideline for both health practitioners and those governmental or expert companies associated with the facility of standards for this kind of healthcare delivery.
Such treatment programs may happen within a discomfort treatment facility, but they are not needed for the assessment and treatment of patients with chronic discomfort. The following terms will be quickly defined in this area; a more complete description of the qualities of each type of center appears in subsequent portions of this report.

Pain unit is a synonym for discomfort treatment center (how oftern does a pain management clinic test your urine). An organization of healthcare experts and standard researchers that includes research, teaching and patient care related to acute and chronic discomfort. This is the biggest and most complicated of the pain treatment centers and ideally would exist as a part of a medical school or mentor medical facility.
Not known Details About How To Become A Certified Pain Clinic
The disciplines of healthcare providers needed is a function of the ranges of patients seen and the healthcare resources of the community. The members of the treatment group must interact with each other on a regular basis, both about particular clients and about overall development. Health care services in a multidisciplinary discomfort center should be integrated and based upon multidisciplinary evaluation and management of the patient.
A health care shipment center staffed by physicians of different specialties and other non-physician health care companies who focus on the diagnosis and management of patients with chronic pain. This kind of center varies from a Multidisciplinary Pain Center only since it does not include research and mentor activities in its routine programs.
A healthcare shipment facility focusing upon the medical diagnosis and management of clients with persistent discomfort. A discomfort clinic may concentrate on specific medical diagnoses or in discomforts related to a particular area of the body. A pain clinic may be big or small but it should never ever be a label for an isolated solo professional.
Some Known Facts About Where North Of Boston Is There A Pain Clinic That Accepts Patients Eith No Insurance.
The lack of interdisciplinary evaluation and management distinguishes this kind of center from a multidisciplinary pain center or clinic. Discomfort clinics can, and need to be motivated to, carry out research, however it is not a required quality of this kind of facility (what pain clinic will give you roxy 15th for back pain). This is a health care facility which uses a specific kind of treatment and does not provide extensive assessment or management.
Such a facility may have several health care companies with various expert training; since of its minimal treatment options and the lack of an incorporated, extensive method, it does not receive the term, multidisciplinary. A multidisciplinary discomfort center (MPC) must have on its staff a range of health care service providers efficient in evaluating and dealing with physical, psychosocial, medical, occupation and social aspects of chronic discomfort.
A minimum of 3 medical specializeds must be represented on the personnel of a follow this link multidisciplinary discomfort center. If one of the physicians is not a psychiatrist, doctors from 2 specializeds and a scientific psychologist are the minimum needed. A multidisciplinary discomfort center should be able to evaluate and deal with both the physical and the psychosocial elements of a patient's complaints.
The Buzz on What I Need For Open A Pain Clinic Office In Ms
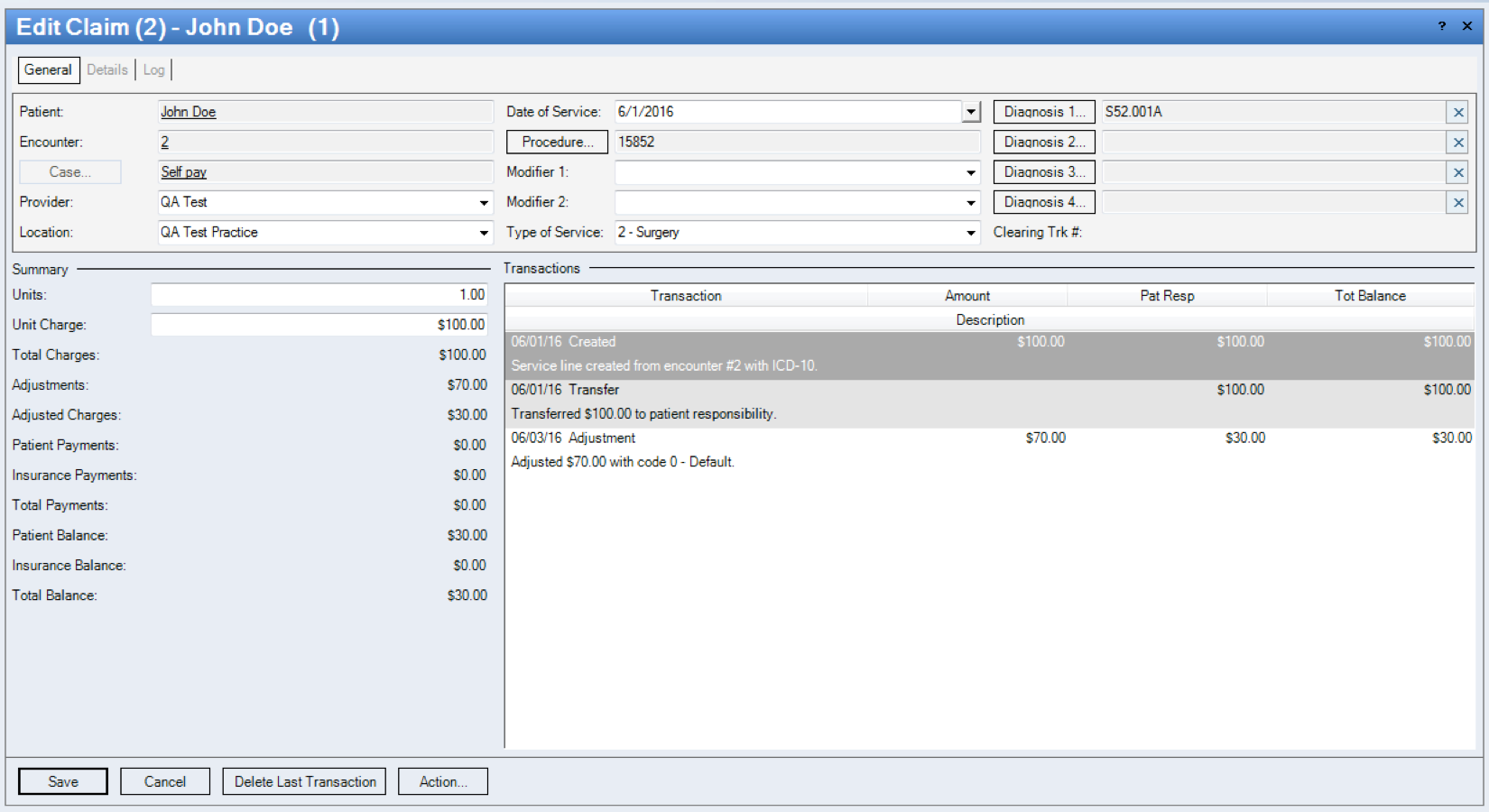
We asked why the charts provided little to no insight regarding the patients' case history, conditions, or treatment strategies. She described that many of the patients experienced lower back or neck discomfort, and without insurance coverage, they couldn't pay for expensive radiology and laboratory tests. She even more explained that, to make the situation worse, the patients grumble loudly and threaten to never come back if there is any attempt to "lower" pain medications.
Chart after chart, the clients were either on oxycodone 30 mg or hydrocodone 10/325 mg, along with a benzodiazepine. When asked if she was aware that these medications, in mix, were potentially hazardous, she with confidence advised me that pain was the fifth crucial sign which many persistent pain patients struggle with stress and anxiety.
She stated she had actually brought a few of her concerns to the practice owner which the owner had ensured her that a compliance program, consisting of urinalysis tests and prescription drug tracking, was on the way. Unfortunately, this circumstance is not fiction. Tipped off by the out-of-date view of discomfort management practices and lack of compliance, we knew that re-education and a compliance program would be the best prescription for this doctor.
The phrase "tablet mill" has actually invaded the typical medical lexicon as a symbol of the Florida pain centers in the early 2000s where prescriptions for high strength opiates were given out thoughtlessly in exchange for money. With a few really restricted exceptions, that does not exist anymore. DEA enforcement and extremely high sentences for drug dealing doctors have all however closed down what we imagine when we hear the words "tablet mill." It has been replaced by a string of prosecutions against physicians who are practicing in an old or irresponsible way and are easily fooled by the modern-day drug dealerships-- patient employers - what depression screening should pain management clinic use.
Top Guidelines Of What Happens If You Fail A Drug Test Pain Clinic
Research studies of doctors who exhibit negligent prescribing habits yield similar outcomes - how to establish a pain management clinic. As a lawyer dealing with the front lines of the "opioid epidemic," the issue is clear. Finding a doctor who deliberately intends to criminally traffic in narcotics is an uncommon event, but must be punished accordingly. However, the bulk of doctors adding to the opioid epidemic are overworked, under-trained doctors who could gain from increased education and training.
Federal district attorneys have just recently received increased funding to buy more hammers-- a lot of hammers. In March 2018, Congress licensed $27 billion in funding to fight the opioid epidemic. The biggest line item in the 2018 budget plan was $15.6 billion in police funding. It is disappointing to see that essentially none of this extra financing will be spent on solving the real problem, which is physician education.

Rather, regulators have actually concentrated on extreme policies and statutes developed to restrict recommending practices. Instead of utilizing alternative enforcement mechanisms, regulators have actually mostly used two methods to fight improper prescribing: licensure cancellation and prosecution. Re-education is not on the menu. Fueled by the 2016 CDC standards, nearly every state has released opioid recommending guidelines, and some have actually taken the extreme action of setting up prescribing limits.
If a state trusts a doctor with a medical license, it should also trust him or her to exercise good judgment and excellent faith in the course of dealing with legitimate patients. Regrettably, doctors are progressively scared to exercise their judgment as wave after wave of recommending guidelines, statutes, and guidelines make compliance progressively tough.
How To Set Up A Pain Management Clinic Things To Know Before You Buy
Ronald W. Chapman II, Esq., is a shareholder at Chapman Law Group, a multistate healthcare law company. He is a defense Additional reading attorney concentrating on healthcare scams and physician over-prescribing cases as well as related OIG and DEA administrative procedures. He is a previous U.S. Marine Corps judge advocate and was previously released to Afghanistan in support of Operation Enduring Freedom.
Patients generally discover it handy to know something about these different types of centers, their different types of treatments, and their relative degree of efficiency. By a lot of traditional healthcare requirements, there are typically four types of clinics that treat discomfort: Clinics that focus on surgeries, such as back fusions and laminectomies Clinics that concentrate on interventional procedures, such as epidural steroid injections, nerve blocks, and implantable gadgets Centers that focus on long-term opioid (i.e., narcotic) medication management Centers that focus on persistent pain rehabilitation programs Often, centers combine these approaches.
Other times, surgeons and interventional discomfort physicians integrate their efforts and have clinics that offer both surgeries and interventional procedures. However, it is traditional to think of centers that treat pain along these 4 classifications surgeries, interventional procedures, long-lasting opioid medications, and chronic pain rehabilitation programs. The fact that there are various types of discomfort centers is a sign of another crucial truth that patients must know (what to expect at a pain management clinic).
Clients with chronic neck or pain in the back frequently look for care at spinal column surgery clinics. While spine surgeries have actually been carried out for about a century for conditions like fractures of the vertebrae or other types of spine instability, spine surgical treatments for the purpose of chronic pain management started about forty years back.
Unknown Facts About What Happens When You Are Referred To A Pain Clinic
A laminectomy is a surgery that removes part of the vertebral bone. A discectomy is a surgical treatment that removes disc material, typically after the disc has actually herniated. A fusion is a surgical procedure that joins several vertebrae together with the usage of bone taken from another area of the body or with metallic rods and screws.
While acknowledging that spine surgeries can be useful for some clients, a good spine surgeon should correct this misunderstanding and state that spine surgical treatments are not cures for persistent spine-related pain. Most of the times of persistent back or neck discomfort, the objective for surgical treatment is to either stabilize the spine or reduce discomfort, but not eliminate it altogether for the rest of one's life.
Mirza and Deyo3 evaluated 5 published, randomized clinical trials for combination surgery. Two had significant methodological issues, which avoided them from drawing any conclusions. Among the staying three revealed that blend surgery was exceptional to conservative care. The other two compared combination surgical treatment to a very minimal version of group-based cognitive behavior modification.
In a big scientific trial, Weinstein, et al.,4 compared patients who received surgery with clients who did not get surgical treatment and discovered typically no difference. They followed up with the clients 2 years later on and again discovered no difference between the groups. However, in a later post, they revealed that the surgical patients had less discomfort typically at a four Drug Rehab year follow-up period.

The Greatest Guide To How Long Does It Take To Get An Appointment At A Pain Clinic
Nevertheless, by one-year follow-up, the differences will no longer appear and the degree of pain that clients have is the same whether they had surgery or not. 6 Reviews of all the research study conclude that there is only minimal evidence that lumbar surgeries are effective in minimizing low back pain7 and there is no proof to recommend that cervical surgeries are effective in decreasing neck pain.8 Interventional discomfort centers are the latest type of pain clinic, coming to be quite common in Drug Rehab Facility the 1990's.
What Is A Pain Clinic Uk Fundamentals Explained
Considering that numerous types of persistent discomfort might need a complex treatment plan along with specialized interventional strategies, discomfort professionals today need to have more training than in the past, and you must discover how your discomfort physician was trained and whether she or he has board accreditation in discomfort management.
A lot of fellowship programs are related to anesthesiology residency training programs. There are likewise fellowship programs related to neurology and physical medication and rehab residency programs. The fellowship consists of at least one year of training in all elements of pain management after conclusion residency training. When a physician has actually become board licensed in their main specialized and has finished a recognized fellowship, they end up being qualified for subspecialty board certification in pain management by the American Board of Anesthesiology, The American Board of Psychiatry and The American Board of Neurology, or the American Board of Physical Medication and Rehabilitation.
In addition to finding out about your pain doctors training and board certification, you likewise ought to ask whether they have experience with your specific discomfort condition and what kinds of treatments they provide (what is a pain clinic uk). Do they only carry out treatments or do they use a multidisciplinary approach to discomfort management? Who do they describe for other treatment alternatives such as surgery, psychological assistance or alternative treatments? How can they be reached if questions or problems occur? What is their total viewpoint of discomfort management? The finest method to be described a pain management specialist is through your main care https://diigo.com/0iro50 doctor.

The 8-Minute Rule for What To Do When Pain Clinic Does Not Prescribe Meds You Need
Clients are likewise often referred by professionals who handle various types of discomfort issues. Back surgeons, neurologists, cancer physicians, along with other experts usually work routinely with a pain physician and can refer you to one. On your first visit to a discomfort management professional, he or she will be familiar with you and start to evaluate your specific discomfort problem.
The questions you are asked and the physical exam will focus on your specific issue, however your pain physician will need to know about previous and existing medical history as well. Typically you will be offered a survey prior to your first check out that will ask detailed concerns about your pain problem, and you will probably be asked to bring any imaging research studies (such as X-rays, computed tomography [CAT] scans, or magnetic resonance imaging [MRI] scans) or other follow this link tests that have actually already been done.
If so, you may require a driver to take you home. Most notably, this see is a chance for your pain doctor to begin to examine all of this brand-new information and discuss with you an initial evaluation of your discomfort issue. He or she may understand precisely what is triggering your discomfort, or maybe more diagnostic treatments will be needed.
Why Did My Pain Clinic Take A Urine Sample for Dummies
A pain center is a healthcare resource that focuses on the medical diagnosis, management and treatment of chronic discomfort. Within numerous centers, professionals that focus on different pain types and conditions are offered. A pain management expert is a medical professional with extra training in the diagnosis and treatment of discomfort.
Pain management professionals prescribe medications, carry out treatments (such as back injections and nerve blocks) and suggest therapies to deal with pain. The first visit to a pain management clinic usually involves a consultation with a general specialist, internist, nurse specialist or medical assistant. The go to usually involves a detailed assessment of the person's discomfort history, a physical examination, pain evaluation, and diagnostic tests.
Depending upon the origin and seriousness of persistent discomfort, an appointment for an assessment with a different discomfort professional within the center may be recommended. Physicians typically available at a pain clinic include the following: General PractitionersInternists NeurologistsRheumatologistsAnesthesiologistsOrthopedistsPhysiatristsPsychiatristsOther specialists at a discomfort clinic may consist of physiotherapists, physical therapists, chiropractic doctors, acupuncturists and psychologists.
What Does The Brighton Pain Clinic In Portland Do Fundamentals Explained
These guidelines are for historic referral just. IASP embraced the Recommendations for Discomfort Treatment Providers in May 2009. IASP believes that clients throughout the world would take advantage of the facility of a set of desirable qualities for pain treatment centers. The concepts set forth in this document can serve as a guideline for both health specialists and those governmental or expert organizations associated with the facility of requirements for this type of health care delivery.
Such treatment programs might occur within a pain treatment center, however they are not required for the assessment and treatment of patients with chronic pain. The following terms will be briefly defined in this area; a more total description of the attributes of each type of facility appears in subsequent parts of this report.
Pain system is a synonym for discomfort treatment facility (what is a pain management clinic nhs). An organization of health care professionals and basic researchers that includes research study, mentor and client care related to severe and chronic discomfort. This is the biggest and most intricate of the pain treatment facilities and preferably would exist as a component of Drug Detox a medical school or teaching health center.

Unknown Facts About How To Refer To A Pain Clinic
The disciplines of healthcare service providers required is a function of the ranges of clients seen and the health care resources of the neighborhood. The members of the treatment group need to communicate with each other regularly, both about particular clients and about total development. Healthcare services in a multidisciplinary pain center need to be incorporated and based upon multidisciplinary evaluation and management of the patient.
A health care delivery center staffed by physicians of different specializeds and other non-physician healthcare providers who specialize in the medical diagnosis and management of clients with persistent pain. This type of center differs from a Multidisciplinary Pain Center only due to the fact that it does not consist of research study and mentor activities in its routine programs.
A healthcare shipment center focusing upon the medical diagnosis and management of clients with persistent pain. A discomfort center might concentrate on particular diagnoses or in pains related to a particular area of the body. A pain center might be large or small but it must never be a label for a separated solo professional.
4 Easy Facts About What Is A Pain Clinic Shown
The absence of interdisciplinary evaluation and management identifies this type of facility from a multidisciplinary pain center or clinic. Discomfort clinics can, and ought to be encouraged to, perform research, however it is not a needed attribute of this kind of center (what is pain management clinic). This is a healthcare center which provides a specific type of treatment and does not offer comprehensive evaluation or management.
Such a center may have one or more health care suppliers with different professional training; due to the fact that of its restricted treatment options and the lack of an incorporated, thorough technique, it does not get approved for the term, multidisciplinary. A multidisciplinary discomfort center (MPC) should have on its personnel a variety of health care suppliers capable of assessing and dealing with physical, psychosocial, medical, professional and social aspects of chronic pain.
A minimum of 3 medical specializeds should be represented on the personnel of a multidisciplinary pain center. If one of the physicians is not a psychiatrist, doctors from 2 specializeds and a scientific psychologist are the minimum required. A multidisciplinary pain center should have the ability to examine and deal with both the physical and the psychosocial elements of a patient's problems.
Things about What Happens When You Get Discharged From A Pain Clinic
We asked why the charts offered little to no insight as to the patients' medical history, conditions, or treatment plans. She explained that the majority of the patients experienced lower back or neck pain, and without insurance coverage, they couldn't afford expensive radiology and lab tests. She even more described that, to make the situation worse, the patients grumble loudly and threaten to never come back if there is any effort to "lower" pain medications.
Chart after chart, the clients were either on oxycodone 30 mg or hydrocodone 10/325 mg, in addition to a benzodiazepine. When asked if she was aware that these medications, in mix, were potentially harmful, she confidently reminded me that pain was the fifth vital sign which the majority of persistent pain patients struggle with stress and anxiety.
She stated she had brought some of her issues to the practice owner and that the owner had actually ensured her that a compliance program, consisting of urinalysis tests and prescription drug tracking, was on the way. Drug Rehab Facility Regrettably, this situation is not fiction. Tipped off by the outdated view of discomfort management practices and lack of compliance, we understood that re-education and a compliance program would be the best prescription for this doctor.
The expression "pill mill" has actually invaded the typical medical lexicon as a symbol of the Florida discomfort centers in the early 2000s where prescriptions for high strength opiates were distributed carelessly in exchange for money. With a couple of really restricted exceptions, that does not exist any longer. DEA enforcement and very high sentences for drug dealing physicians have all however closed down what we picture when we hear the words "pill mill." It has actually been changed by a string of prosecutions versus doctors who are practicing in an old-fashioned or irresponsible manner and are easily fooled by the modern drug dealerships-- patient employers - what i need for open a pain clinic office in ms.
What Is The Doctor's Name At Eureka Pain Clinic Can Be Fun For Everyone
Research studies of physicians who exhibit reckless recommending habits yield similar results - clecveland clinic how do i get rid of shingle pain. As a lawyer dealing with the front lines of the "opioid epidemic," the problem is clear. Finding a doctor who deliberately plans to criminally traffic in narcotics is an uncommon event, but need to be punished accordingly. However, the bulk of doctors adding to the opioid epidemic are overworked, under-trained physicians who could gain from increased education and training.
Federal prosecutors have recently gotten increased funding to acquire more hammers-- a great deal of hammers. In March 2018, Congress licensed $27 billion in moneying to fight the opioid epidemic. The biggest line product in the 2018 budget plan was $15.6 billion in police financing. It is disappointing to see that essentially none of this additional funding will be spent on fixing the genuine issue, which is doctor education.
Rather, regulators have actually focused on severe policies and statutes created to limit prescribing practices. Rather than using alternative enforcement systems, regulators have mostly utilized two approaches to fight inappropriate prescribing: licensure cancellation and prosecution. Re-education is not on the menu. Fueled by the 2016 CDC standards, nearly every state has actually released opioid prescribing guidelines, and some have taken the extreme action of instituting recommending limits.
If a state trusts a physician with a medical license, it should likewise trust him or her to work out profundity and good faith in the course of treating legitimate clients. Sadly, physicians are increasingly afraid to exercise their judgment as wave after wave of prescribing standards, statutes, and guidelines make compliance progressively tough.
The What Does A Pain Clinic Do Diaries
Ronald W. Chapman II, Esq., is a shareholder at Chapman Law Group, a multistate healthcare law firm. He is a defense lawyer concentrating on healthcare scams and doctor over-prescribing cases as well as associated OIG and DEA administrative procedures. He is a former U.S. Marine Corps judge supporter and was previously deployed to Afghanistan in assistance of Operation Enduring Liberty.
Clients normally find it helpful to understand something about these different kinds of centers, their various kinds of treatments, and their relative degree of effectiveness. By many standard healthcare requirements, there are generally four kinds of clinics that treat discomfort: Centers that focus on surgical treatments, such as spine blends and laminectomies Centers that focus on interventional treatments, such as epidural steroid injections, nerve blocks, and implantable gadgets Centers that concentrate on long-lasting opioid (i.e., narcotic) medication management Centers that concentrate on persistent pain rehabilitation programs Sometimes, centers integrate these approaches.
Other times, cosmetic surgeons and interventional pain physicians combine their efforts and have clinics that supply both surgical treatments and interventional procedures. Nevertheless, it is standard to consider centers that deal with pain along these 4 classifications surgeries, interventional procedures, long-lasting opioid medications, and persistent discomfort rehabilitation programs. The truth that there are different kinds of discomfort clinics is indicative of another important fact that patients should understand (what pain clinic will give you roxy 15th for back pain).
Patients with persistent neck or pain in the back typically seek care at spine surgery centers. While spinal surgical treatments have actually been carried out for about a century for conditions like fractures of the vertebrae or other forms of spine instability, back surgical treatments for the function of chronic pain management started about forty years ago.
Should You Go To The Walk In Clinic When You Are Having Pain Behind Right Breast for Dummies
A laminectomy is a Drug Rehab surgery that gets rid of part of the vertebral bone. A discectomy is a surgery that removes disc product, typically after the disc has actually herniated. A blend is a surgery that joins one or more vertebrae together with the usage of bone taken from another area of the body or with metallic rods and screws.

While acknowledging that spinal column surgeries can be practical for some patients, a great spinal column surgeon need to correct this misconception and state that spinal column surgical treatments are not cures for persistent spine-related pain. For the most part of persistent back or neck pain, the goal for surgical treatment is to either support the spine or reduce discomfort, but not eliminate it entirely for the rest of one's life.
Mirza and Deyo3 examined five released, randomized scientific trials for fusion surgical treatment. Two had substantial methodological issues, which avoided them from drawing any conclusions. One of the remaining 3 showed that combination surgery was superior to conservative care. The other two compared fusion surgical treatment to a very limited version of group-based cognitive behavioral therapy.
In a big clinical trial, Additional reading Weinstein, et al.,4 compared patients who got surgery with patients who did not get surgical treatment and discovered usually no distinction. They followed up with the clients 2 years later on and once again found no difference between the groups. Nevertheless, in a later short article, they showed that the surgical patients had less discomfort usually at a 4 year follow-up period.
The 8-Minute Rule for What To Expect When You Go To A Pain Clinic
However, by one-year follow-up, the differences will no longer appear and the degree of discomfort that clients have is the same whether they had surgery or not. 6 Evaluations of all the research study conclude that there is just minimal evidence that back surgical treatments are effective in lowering low back pain7 and there is no evidence to recommend that cervical surgeries work in minimizing neck discomfort.8 Interventional discomfort centers are the newest kind of discomfort clinic, becoming rather common in the 1990's.
Not known Details About What Type Pain Left Arm From Top To Elbow Might Indicate Heart Problem
Since lots of types of persistent discomfort may require a complex treatment strategy in addition to specialized interventional methods, pain specialists today need to have more training than in the past, and you need to learn more about how your pain doctor was trained and whether he or she has board accreditation in pain management.
A lot of fellowship programs are related to anesthesiology residency training programs. There are also fellowship programs connected with neurology and physical medication and rehab residency programs. The fellowship includes a minimum of one year of training in all aspects of discomfort management after completion residency training. When a physician has become board certified in their main specialty and has finished a certified fellowship, they become qualified for subspecialty board certification in discomfort management by the American Board of Anesthesiology, The American Board of Psychiatry and The American Board of Neurology, or the American Board of Physical Medicine and Rehab.
In addition to finding out about your pain doctors training and board accreditation, you likewise should ask whether they have experience with your specific pain condition and what types of treatments they offer (how oftern does a pain management clinic test your urine). Do they just carry out treatments or do they utilize a multidisciplinary approach to discomfort management? Who do they describe for other treatment alternatives such as surgery, mental assistance or alternative therapies? How can they be reached if concerns or problems develop? What is their general philosophy of discomfort management? The very best way to be referred to a discomfort management professional is through your medical care doctor.
See This Report about Sports Medicine Clinic For Pain When Running
Patients are likewise typically referred by specialists who handle different kinds of pain issues. Back cosmetic surgeons, neurologists, cancer doctors, as well as other experts usually work regularly with a discomfort physician and can refer you to one. On your very first follow this link visit to a discomfort management professional, he or she will learn more about you and start to examine your particular pain issue.
The questions you are asked and the physical exam will concentrate on your specific issue, but your pain physician will need to know about past and present case history as well. Frequently you will be provided a survey prior to your first visit that will ask comprehensive concerns about your pain problem, and you will most likely be asked to bring any imaging studies (such as X-rays, calculated tomography [FELINE] scans, or magnetic resonance imaging [MRI] scans) or other tests that have actually already been done.
If so, you may require a chauffeur to take you house. Most significantly, this visit is a chance for your discomfort physician to start to examine all of this new information and go over with you an initial evaluation of your discomfort problem. He or she may understand precisely what is causing your pain, or perhaps more diagnostic treatments will be https://diigo.com/0iro50 required.
The Only Guide for How Does A Pain Management Clinic Help People
A discomfort clinic is a healthcare resource that concentrates on the diagnosis, management and treatment of chronic discomfort. Within numerous centers, professionals that concentrate on various discomfort types and conditions are offered. A discomfort management professional is a medical professional with additional training in the medical diagnosis and treatment of discomfort.

Discomfort management professionals prescribe medications, carry out procedures (such as back injections and nerve blocks) and advise therapies to deal with discomfort. The very first check out to a pain management clinic normally includes a visit with a basic specialist, internist, nurse practitioner or medical assistant. The check out usually involves a comprehensive evaluation of the individual's pain history, a physical test, pain assessment, and diagnostic tests.
Depending upon the origin and severity of persistent pain, a consultation for a consultation with a different pain expert within the center might be suggested. Physicians usually available at a discomfort clinic consist of the following: General PractitionersInternists NeurologistsRheumatologistsAnesthesiologistsOrthopedistsPhysiatristsPsychiatristsOther professionals at a pain clinic might consist of physical therapists, occupational therapists, chiropractic doctors, acupuncturists and psychologists.
The 5-Minute Rule for Sports Medicine Clinic For Pain When Running

These standards are for historic recommendation only. IASP embraced the Recommendations for Pain Treatment Services in May 2009. IASP thinks that clients throughout the world would gain from the establishment of a set of preferable attributes for discomfort treatment facilities. The principles stated in this file can act as a standard for both health specialists and those governmental or expert organizations associated with the facility of standards for this kind of healthcare shipment.
Such treatment programs may take place within a pain treatment center, however they are not needed for the evaluation and treatment of clients with chronic pain. The following terms will be briefly defined in this section; a more complete description of the characteristics of each type of facility appears in subsequent portions of this report.
Discomfort system is a synonym for pain treatment facility (who are the pa's and np's at sanford pain clinic). A company of health care specialists and fundamental scientists that includes research study, teaching and client care associated to intense and chronic pain. This is the largest and most complex of the discomfort treatment facilities and ideally would exist as a part of a medical school or mentor healthcare facility.
Excitement About What Is A Pain Clinic
The disciplines of healthcare service providers needed is a function of the varieties of clients seen and the healthcare resources of the community. The members of the treatment team must communicate with each other on a routine basis, both about specific patients and about general advancement. Health care services in a multidisciplinary discomfort clinic need to be integrated and based upon multidisciplinary evaluation and management of the client.
A healthcare delivery facility staffed by doctors of different specializeds and other non-physician healthcare providers who specialize in the medical diagnosis and management of patients with persistent discomfort. This kind of facility differs from a Multidisciplinary Pain Center only due to the fact that it does not include research study and mentor activities in its routine programs.
A health care shipment facility focusing upon the diagnosis and management of clients with persistent discomfort. A discomfort center might concentrate on specific medical diagnoses or in pains connected to a specific area of the body. A pain clinic might be large or small but it needs to never ever be a label for an isolated solo specialist.
The Definitive Guide for What Pain Clinic Will Give You Roxy 15th For Back Pain
The lack of interdisciplinary assessment and management identifies this type of center from a multidisciplinary pain center or clinic. Discomfort centers can, and need to be encouraged to, Drug Detox perform research study, however it is not a required quality of this type of facility (how long do you need to be off antibiotics before pain clinic shots). This is a health care center which provides a specific type of treatment and does not offer extensive assessment or management.
Such a center might have several healthcare companies with various professional training; due to the fact that of its limited treatment options and the absence of an integrated, extensive technique, it does not certify for the term, multidisciplinary. A multidisciplinary discomfort center (MPC) should have on its personnel a range of health care providers capable of examining and treating physical, psychosocial, medical, vocational and social elements of chronic discomfort.
A minimum of three medical specialties need to be represented on the personnel of a multidisciplinary pain center. If one of the doctors is not a psychiatrist, doctors from two specialties and a scientific psychologist are the minimum needed. A multidisciplinary pain center must be able to examine and treat both the physical and the psychosocial aspects of a client's grievances.
The What Kind Of Ortho Clinic Do You See For Hip Pain Ideas
We asked why the charts offered little to no insight as to the patients' case history, conditions, or treatment strategies. She discussed that many of the patients struggled with lower back or neck discomfort, and without insurance coverage, they couldn't afford costly radiology and laboratory tests. She even more explained that, to make the scenario even worse, the clients complain loudly and threaten to never ever return if there is any effort to "lower" discomfort medications.
Chart after chart, the patients were either on oxycodone 30 mg or hydrocodone 10/325 mg, together with a benzodiazepine. When asked if she knew that these medications, in combination, were possibly harmful, she with confidence advised me that pain was the fifth essential indication which a lot of persistent discomfort patients struggle with anxiety.
She stated she had actually brought a few of her concerns to the practice owner and that the owner had actually ensured her that a compliance program, consisting of urinalysis tests and prescription drug monitoring, was on the method. Unfortunately, this situation is not fiction. Tipped off by the outdated view of discomfort management practices and lack of compliance, we knew that re-education and a compliance program would be the ideal prescription for this physician.
The expression "tablet mill" has gotten into the common medical lexicon as a sign of the Florida pain clinics in the early 2000s where prescriptions for high strength opiates were handed out carelessly in exchange for money. With a few really restricted exceptions, that does not exist any longer. DEA enforcement and exceptionally high sentences for drug dealing doctors have all however closed down what we imagine when we hear the words "pill mill." It has actually been changed by a string of prosecutions against doctors who are practicing in an old or negligent way and are easily fooled by Additional reading the contemporary drug dealerships-- patient Drug Rehab Facility employers - why is cps pain clinic closing.
Facts About Why Is Taking So Long To Get In The New Pain Clinic Revealed
Research studies of doctors who display careless recommending habits yield comparable results - what does a pain clinic drug test for. As an attorney dealing with the front lines of the "opioid epidemic," the issue is clear. Finding a doctor who deliberately plans to criminally traffic in narcotics is an uncommon event, however must be punished accordingly. However, the bulk of physicians adding to the opioid epidemic are overworked, under-trained physicians who could benefit from increased education and training.
Federal district attorneys have recently received increased funding to purchase more hammers-- a great deal of hammers. In March 2018, Congress authorized $27 billion in moneying to fight the opioid epidemic. The biggest line product in the 2018 budget was $15.6 billion in police financing. It is frustrating to see that essentially none of this extra funding will be invested on fixing the real issue, which is doctor education.
Instead, regulators have actually concentrated on heavy-handed policies and statutes designed to restrict recommending practices. Instead of using alternative enforcement mechanisms, regulators have actually mostly used two techniques to fight inappropriate prescribing: licensure revocation and prosecution. Re-education is not on the menu. Fueled by the 2016 CDC standards, almost every state has issued opioid recommending standards, and some have taken the drastic action of setting up recommending limitations.
If a state trusts a doctor with a medical license, it should likewise trust him or her to work out profundity and good faith in the course of treating legitimate patients. Regrettably, doctors are progressively afraid to exercise their judgment as wave after wave of recommending guidelines, statutes, and rules make compliance significantly hard.
Fascination About How Can You Sue A Pain Clinic

Ronald W. Chapman II, Esq., is a shareholder at Chapman Law Group, a multistate health care law company. He is a defense lawyer focusing on healthcare fraud and physician over-prescribing cases in addition to associated OIG and DEA administrative procedures. He is a previous U.S. Marine Corps judge advocate and was previously deployed to Afghanistan in assistance of Operation Enduring Liberty.
Patients typically find it practical to know something about these various kinds of centers, their various kinds of treatments, and their relative degree of effectiveness. By most standard health care requirements, there are normally 4 kinds of centers that treat discomfort: Centers that concentrate on surgeries, such as spinal blends and laminectomies Centers that concentrate on interventional treatments, such as epidural steroid injections, nerve blocks, and implantable gadgets Clinics that focus on long-lasting opioid (i.e., narcotic) medication management Clinics that focus on persistent pain rehab programs Sometimes, centers combine these methods.
Other times, cosmetic surgeons and interventional discomfort doctors integrate their efforts and have clinics that provide both surgeries and interventional procedures. Nevertheless, it is traditional to think of clinics that deal with discomfort along these 4 categories surgeries, interventional treatments, long-lasting opioid medications, and chronic pain rehab programs. The truth that there are various kinds of pain centers is a sign of another essential truth that clients should know (how to open a pain management clinic in florida).
Clients with persistent neck or pain in the back frequently look for care at spine surgery centers. While spinal surgical treatments have actually been performed for about a century for conditions like fractures of the vertebrae or other kinds of spinal instability, spinal surgical treatments for the function of persistent pain management started about forty years ago.
What Is The Estimated Cost To Building A Free-standing 8 Hour A Day Pain Clinic Things To Know Before You Get This
A laminectomy is a surgery that eliminates part of the vertebral bone. A discectomy is a surgical procedure that removes disc product, typically after the disc has herniated. A combination is a surgical procedure that signs up with one or more vertebrae together with using bone taken from another location of the body or with metallic rods and screws.
While acknowledging that spine surgeries can be practical for some clients, a good spine cosmetic surgeon should fix this misunderstanding and state that spine surgical treatments are not remedies for chronic spine-related pain. Most of the times of chronic back or neck pain, the goal for surgical treatment is to either stabilize the spine or reduce pain, but not eliminate it altogether for the rest of one's life.
Mirza and Deyo3 reviewed 5 released, randomized medical trials for fusion surgery. Two had considerable methodological issues, which avoided them from drawing any conclusions. One of the remaining three showed that fusion surgery transcended to conservative care. The other 2 compared fusion surgery to a very restricted version of group-based cognitive behavioral therapy.
In a large clinical trial, Weinstein, et al.,4 compared clients who received surgery with patients who did not receive surgical treatment and discovered on typical no distinction. They followed up with the patients two years later on and once again discovered no distinction between the groups. Nevertheless, in a later post, they revealed that the surgical clients had less pain on average at a 4 year follow-up period.
Get This Report about How To File Drug Rehab Complaint Against Pain Clinic
Nevertheless, by 1 year follow-up, the distinctions will no longer appear and the degree of pain that patients have is the same whether they had surgical treatment or not. 6 Evaluations of all the research study conclude that there is only minimal evidence that back surgeries are effective in lowering low back pain7 and there is no evidence to suggest that cervical surgical treatments are efficient in decreasing neck pain.8 Interventional pain centers are the most recent kind of discomfort clinic, coming to be quite typical in the 1990's.
An Unbiased View of How To Get A Referral To A Pain Clinic
You do not require a lawyer, however if you have one, make the most of his recommendations - how to establish a pain management clinic. The forms themselves are basic and straightforward and are offered on your state's website. You can also order them by phone. Make your complaint more effective by composing a clear declaration.
of what happened to you and any troubles that you are having in discovering another physician. It might assist if you number each paragraph and inform your story chronologically. If possible, have someone else read it to ensure it seems clear (who are the pa's and np's at sanford pain clinic). Do not feel limited by a type that does not allow much area for your remarks. Describe the emotional and physical impact of the termination. Make it clear if he was verbally abusive! Connect quick statements by anyone who has observed the.
effect.
that the termination has actually had on you and any other files that may help the board understand that you are a genuine discomfort client with a severe medical condition. If you wish to follow up with the board, talk with the clerk to make sure it was put on the docket. Answer any questions and ask to be kept notified of case progress. Abandonment is a tort( legal incorrect) that might give you trigger for a legal action versus your physician. To show desertion you typically need to show (a) a physician-patient relationship;( b )that was terminated or overlooked by the doctor and (c) that triggered you harm.
In addition, there is a tort called" infliction of serious psychological distress," which requires (a) an Drug Rehab Facility action taken by the offender (b) which was reasonably foreseeable to cause extreme distress; and (c) that it did in reality cause extreme psychological distress. Some states require a physical injury, but there is some precedent that acknowledges pain as such.

The 8-Second Trick For Where Is The Pain Clinic In Morristown
If the defendant doctor knew and meant to cause the emotional damage, a more serious tort is conjured up. The requirements of these torts are often complicated and you should discuss your state's precedents with your attorney. Do not take a fit gently and do not expect a windfall. Lawsuits is very hard on anybody with a persistent disease and much more so with.
RSD due to the fact that of the stress involved. If you can not pay for to pay an attorney, you will need to convince one that the case is worth taking on a contingency basis; experience has proven this hard. A lot of attorneys know extremely little about opioids and even less about discomfort management. You will require to educate your attorney so that he can examine your case smartly. For a printcopy, contact the RSDSA office at( 877 )662-7737. 1. AMA Ethical Declaration 2.1, made effective for chronicpain by the Council on Ethical and Judicial Affairs in 2002. Are you sure you aren't lying, though?Let's say you have actually been experiencing discomfort for a while, perhaps years. Believing, ever so naively, that remaining in constant pain for months on end isn't normal, you go to your doctor.
He buys blood work and perhaps an X-ray or a sonogram. All results return normal, Addiction Treatment Center so your medical professional dismisses your issues. I get it. It took me 32 years to get a medical professional to take my discomfort seriously and to get a diagnosis with a connective tissue disease I was born with that no physician ever saw my obvious symptoms of, whoops. http://judahktxy149.huicopper.com/cleveland-clinic-pain-at-bottom-of-sternum-when-i-go-go-sleep-can-be-fun-for-anyone I don't desire you to wait years for responses, though. 1. Say" I am in discomfort." Be ignored or dismissed, since it can't be that bad. Entrust to your tail between your legs, you wascally wabbit. 2. Say" I am in extreme.
pain." This time your doctor will react! With an eye roll. Followed by a reminder that all your blood work is negative and you don't" look sick." Leave the medical professional's workplace, you remarkable exaggerator, you! 3. Bring a polygraph maker to your next visit. Make sure you're hooked up to it when you remind your doc that you're in severe, day-to-day discomfort. He'll acknowledge that while.
the maker claims you aren't lying, your insurance coverage doesn't cover polygraph tests, and therefore, he can't take the outcomes into account when identifying your treatment plan, which is yoga. When your physician recommends yoga, solemnly inform him that your discomfort is so bad you can't even do yoga.
Some Known Questions About How To Open A Pain Management Clinic In Florida.
So, if he might just assist with this extensive joint and muscle pain that is slowly, gradually debilitating you a growing number of weekly whether that be physical treatment or discomfort meds or a specialist or just, you understand, something you assure to take a yoga class. Write a guide called "A 30 Second Guide on Standard Human Decency" and anonymously mail it to your medical professional.
the week before your consultation. He will not read it that is the dilemma of the decency guide. 7. Get your hands on a traffic control costume. Eliminate two red felt circles and stitch them over the yellow and thumbs-ups. The doctor will take in your costume of 3 traffic signals and begin to ask "Why?" This is when you chime in with, "Why are they all.
stop lights? Thankful you asked! So you'll STOP disregarding my pain." 8. Bring your corgi for compassion since that clever pup with those huge brown eyes can get any human to do anything for her, up to and consisting of persuading medical specialists to take her mother's discomfort seriously. 9. Dress like a clown. Cry, weep your big, unfortunate clown tears." Doc, "you'll plead, "they state clowns only cry in secret. But take a look at me go!" Your medical professional will detect you with" Crocodile Tear-Itis "and most likely offer you a psych referral before formally dropping you from his practice. That night you'll ponder in your rocking chair, still outfitted in your clown costume, muttering to yourself as you attempt to determine where it all.
failed, "But everybody enjoys a clown." 10. Or get among those novelty buzzers your elementary school teachers hated and shock him when he shakes your hand. When he screams, describe," Now you understand how I feel! Let's talk pain management solutions." 11. Get your partner or a friend to come with you using a transformed "I'm With Dumb" shirt so it states," I'm with My Loved One Who Is Suffering and I Want You to Listen to Her and Stop Making Her Life Harder. what does a pain clinic drug test for." Ensure they position themselves so that the arrow indicate you. Go to medical school and become a physician, figure out the source of your discomfort, cure it with an outrageous, gimmicky, revolutionary, Nobel Prizewinning brand-new treatment. You're now pain-free, but don't lose focus! Ensure you rub it in your physician's face and always remember that you didn't do all this to cure your pain, but to spite him. what is a pain clinic and what do they do. Die in front of your physician, with fingers crossed( to increase the possibilities of resuscitating you.
). If you do not pass away, he will probably say you were exaggerating. If you pass away, congratulations! Your pain was real, you were really ill, and everybody who doubted you is extremely sorry. We want you great deals of success in the afterlife.
Everything about Where North Of Boston Is There A Pain Clinic That Accepts Patients Eith No Insurance
Michael J - what happens if you fail a drug test at a pain clinic. Cousins, and chaired by Learn more the Secretary of IASP, Dr. John D. Loeser. John D. Loeser, Mental Health Facility MD, USA, - where north of boston is there a pain clinic that accepts patients eith no insurance.

ChairmanFrancois Boureau, MD, PhD, FrancePeter Brooks, Additional reading MBBS, MD, FRACP, FRACM, AustraliaTeresa Ferrer-Brechner, MD, USAHoward L. Fields, MD, PhD, USACorey D. Fox, PhD, USAHans U. Gerbershagen, MD, GermanyMartin Grabois, MD, USADouglas M. Little, MBBS, FFARCS, AustraliaGeorge Mendelson, MBBS, MD, FRANZCP, AustraliaIsaac Pinter, PhD, USARussell K. Portenoy, MD, USARobyn J. where is the pain clinic in morristown. Quinn, RMN, AustraliaHoward L. Rosner, MD, USAJohn C. Rowlingson, MD, USABengt H. Sjolund, MD, PhD, SwedenPeter J. Vicente, PhD, USAC. Peter N. Watson, MD, CanadaMichael Wood, PhD, Australia. Pain management physicians physicians who focus on the assessment, diagnosis, and treatment of pain have actually advanced training that qualifies them as your best source of treatment if you are experiencing any kind of discomfort due to illness or injury. After a general residency, these doctors undergo an extra 1 year fellowship in pain management, and they are board-certified in a specialized, such as sport injuries or cancer discomfort.
How To Become A Certified Pain Clinic - The Facts
Michael J - what was the first pain management clinic. Cousins, and chaired by the Secretary of IASP, Dr. John D. Loeser. John D. Loeser, MD, USA, - what pain clinic will give you roxy 15th for back pain.
ChairmanFrancois Boureau, MD, PhD, FrancePeter Brooks, MBBS, MD, FRACP, FRACM, AustraliaTeresa Learn more Ferrer-Brechner, MD, USAHoward L. Fields, MD, PhD, USACorey D. Fox, PhD, USAHans U. Gerbershagen, Mental Health Facility MD, GermanyMartin Grabois, MD, USADouglas M. Little, MBBS, FFARCS, AustraliaGeorge Mendelson, MBBS, MD, FRANZCP, AustraliaIsaac Pinter, PhD, USARussell K. Portenoy, MD, USARobyn J. what was the first pain management clinic. Quinn, RMN, AustraliaHoward L. Rosner, MD, USAJohn C. Rowlingson, MD, USABengt H. Sjolund, MD, PhD, SwedenPeter J. Vicente, PhD, USAC. Peter N. Watson, MD, CanadaMichael Wood, PhD, Australia. Pain management medical professionals doctors who specialize in the assessment, diagnosis, and treatment of discomfort have actually advanced Additional reading training that qualifies them as your finest source of treatment if you are experiencing any kind of pain due to illness or injury. After a basic residency, these physicians undergo an additional one-year fellowship in discomfort management, and they are board-certified in a specialized, such as sport injuries or cancer pain.
Where Is Allegeny Pain Management Clinic Things To Know Before You Get This
Michael J - what happens if you fail a drug test at a pain clinic. Cousins, and chaired by the Secretary of IASP, Dr. John D. Loeser. John D. Loeser, MD, U.S.A., - where is northoaks pain management clinic.

ChairmanFrancois Boureau, MD, PhD, FrancePeter Brooks, MBBS, MD, FRACP, FRACM, AustraliaTeresa Ferrer-Brechner, MD, USAHoward L. Fields, MD, PhD, USACorey D. Fox, PhD, USAHans U. Gerbershagen, MD, GermanyMartin Grabois, MD, USADouglas M. Little, MBBS, FFARCS, AustraliaGeorge Mendelson, MBBS, MD, FRANZCP, AustraliaIsaac Pinter, PhD, USARussell K. Portenoy, MD, USARobyn J. what happens at a pain management clinic. Quinn, RMN, AustraliaHoward L. Rosner, MD, USAJohn C. Rowlingson, MD, USABengt H. Sjolund, MD, PhD, SwedenPeter J. Vicente, PhD, USAC. Peter N. Watson, MD, Learn more CanadaMichael Wood, PhD, Australia. Discomfort management physicians physicians who focus on the assessment, medical diagnosis, and treatment of pain have advanced training Additional reading that qualifies them as your Mental Health Facility finest source of treatment if you are experiencing any kind of pain due to disease or injury. After a basic residency, these doctors go through an extra one-year fellowship in discomfort management, and they are board-certified in a specialty, such as sport injuries or cancer discomfort.
4 Easy Facts About Pain Clinic What If You Are Short On Oxycodone Shown
The listing will provide an address and contact number (in addition to any disciplinary actions assigned to the physician). A group of local discomfort experts, the, have come together to help in the occasion a discomfort clinic all of a sudden closes and patients find themselves unexpectedly without access to care or guidance.
However, the group thinks that we need to come together as a neighborhood to assist our neighbors when they, by no fault of their own, all of a sudden discover themselves medically orphaned due to the abrupt closure of their discomfort center. Kentuckiana toll totally free number: Keep in mind: This toll complimentary number is not manned.
It is not a basic recommendation service for clients. And there is no assurance you will get a call back. If you think you may have a medical emergency, call your doctor, go to the emergency situation department, or call 911 right away. This blog site post will be upgraded with, lists, contact number, and extra resources when new details appears.
And don't give up hope. This scenario might be tough, however it might likewise be a possibility for a brand-new beginning. * Note: All clinicians need to recognize with the details in Part One (above) as this is what your patients read. Medical care practices will likely take on most of connection of care concerns caused by the abrupt closure of a large pain clinic.
3 questions become vital: Do you continue the present regimen? Do you change the program (e.g. taper or design a brand-new strategy)? Do you decide not to prescribe any medications and deal with the withdrawal? The responses to these questions can just come from the specific care supplier. Naturally, we want to relieve suffering.

Excitement About What Does A Pain Clinic Drug Test Test For
Some prescribers might feel comfortable with greater dosages and specialized formulations of medications. Others may be ready to recommend (within a narrower set of personal borders) frequently prescribed medications with which they have familiarity. And there will be some clinicians who truthfully feel they are not geared up (i.e. training, experience, manpower) to recommend controlled compounds at all.
Let's begin with some advice from the Washington State Department of Health (a leader in resolving opioid recommending problems): Clinicians ought to empathically review benefits and risks of ongoing high-dosage opioid therapy and deal to deal with the client to taper opioids to lower does. Professionals keep in mind that clients tapering opioids after taking them https://central.newschannelnebraska.com/story/42268615/addiction-treatment-center-offers-guidance-on-selecting-the-right-rehab-center for several years may need very slow opioid tapers in addition to stops briefly in the taper to enable progressive accommodation to lower opioid does - my hospital is charging me 1727.00 for a urine test when i see pain clinic.
The U.S. Centers for Illness Control and Avoidance particularly advises against rapid taper for people taking more than 90 mg MEDICATION each day. Clinicians need to evaluate clients on more than 90 mg MED or who are on combination treatment for overdose risk. Prescribe or offer naloxone. More on this topic is in the New England Journal of Medicine.
Pharmacist keeping in mind various withdrawal metrics: Often a lower dose than they are accustomed to taking will suffice. for treating opioid withdrawal is to calculate the client's (morphine comparable day-to-day dosage) and after that supply the patient with a portion of this MEDD (e.g. 80-90%), in the type of immediate release medication, for a couple of days and then re-evaluate.
Instead the clinician may prescribe opioids with which he or she feels more comfortable (i.e. Percocet rather of Oxycontin) and still treat the client's withdrawal efficiently. Fortunately, there are a variety of well-vetted protocols to guide us. An effective plan of care is born of understanding about the client (e.g.
Getting My Sports Medicine Clinic For Pain When Running To Work
The Mayo Clinic published a fantastic standard guide on opioid tapering: And the Washington State Firm Medical Directors' Group has a really nice step-by-step guide to tapering: For primary care providers who do not desire to write the medications, they may have to deal with dealing with withdrawal. I found an outstanding and simple to use guide to dealing with opioid withdrawal in (and other medications in other chapters) from the As kept in mind above in Part One, the has actually published a succinct "pocket guide" to tapering.
Ref: https://www.cdc - what is the doctor's name at eureka pain clinic.gov/drugoverdose/pdf/clinical_pocket_guide_tapering-a.pdf Reasonably, even the most diligent tapering plans can fizzle, and withdrawal symptoms of differing seriousness can happen. Also, as stated above, some clinicians will make the choice to prescribe any controlled compounds in treatment of their patients' withdrawal. In either instance, clinicians need to be familiar with what is offered (over-the-counter in addition to by prescription) to treat withdrawal signs.
And for those clinicians interested a few of the more intense pharmacologic techniques to treating withdrawal, consider this article from Dialogues in Clinical Neuroscience: Excerpts:: The antihypertensive, 2-adrenergic agonist drug clonidine has been used to assist in opioid withdrawal in both inpatient and outpatient settings for over 25 years.18 21 It works by binding to 2 autoreceptors in the locus coeruleus and suppressing its hyperactivity throughout withdrawal.
Dropouts are more likely to take place https://www.wrde.com/story/42174669/new-podcast-and-video-help-addicts-find-a-great-hialeah-fl-treatment-center early with clonidine and later on with methadone. In a research study of heroin cleansing, buprenorphine did much better on retention, heroin use, and withdrawal severity than the clonidine group.12 Because clonidine has moderate analgesic impacts, included analgesia may not be needed during the withdrawal period for medical opioid addicts.
Lofexidine, an analogue of clonidine, has been authorized in the UK and may be as reliable as clonidine for opioid withdrawal with less hypotension and sedation.23,24 Integrating lofexidine with low-dose naloxone appears to enhance retention signs and time to relapse. Helpful procedures: Sleeping disorders is both typical and debilitating. Clonazepam, trazodone, and Zolpidem have actually all been utilized for withdrawal-related sleeping disorders, however the choice to use a benzodiazepine requires to be made thoroughly, specifically for outpatient cleansing. Minerals and vitamin supplements are frequently provided.
How To Get Into A Pain Clinic In Ohio - The Facts
A note on policies: When prescribing, keep in mind that Kentucky now has actually enforced a three-day limit for treatment of intense conditions with Set up II controlled compounds. If your client has persistent pain, and your treatment addresses this chronic condition, then the three-day limit should not use. Here is the language in Kentucky's pain guidelines: In addition to the other requirements developed in this administrative regulation, for functions of dealing with discomfort as or associated to an acute medical condition, a physician shall not recommend or dispense more than a three (3 )day supply of a Set up II illegal drug, unless the physician identifies that more than a 3 (3) day supply is clinically essential and the physician documents the acute medical condition and absence of alternative medical treatment choices to justify the amount of the illegal drug recommended or given. The mnemonic" Strategy to THINK" (see below) can assist doctors remember what Kentucky needs in order to at first prescribe illegal drugs for chronic discomfort: Document a strategy() that discusses why and how the illegal drug will be used. Teach() the client about appropriate storage of the medications and when to stop taking them (where is the pain clinic in morristown).